Uganda Critical Care Training: An Interview with Dr. Fred Bulamba
An Interview with Dr. Fred Bulamba
An Interview with Dr. Fred Bulamba
The Government of Uganda is undertaking an ambitious effort to increase critical care capacity by fully equipping ICUs at all regional referral hospitals across the nation. We’re proud the Gradian Comprehensive Care Ventilator (Gradian CCV) and our model of training and bio-medical support can serve this critical moment and the partners on the frontlines, such as the Association of Anesthesiologists of Uganda (AAU) and Joint Medical Store (JMS)—a leading medical device and pharmaceutical distributor—making this change a reality for the nation’s COVID-19 response and future health system strength.
The AAU and JMS recently produced a series of short video interviews with anesthesiologists and intensive care specialists about the current state and future vision of critical care in Uganda and what it’ll take to get there, from policy to equipment to education and tackling the biggest challenges to progress.
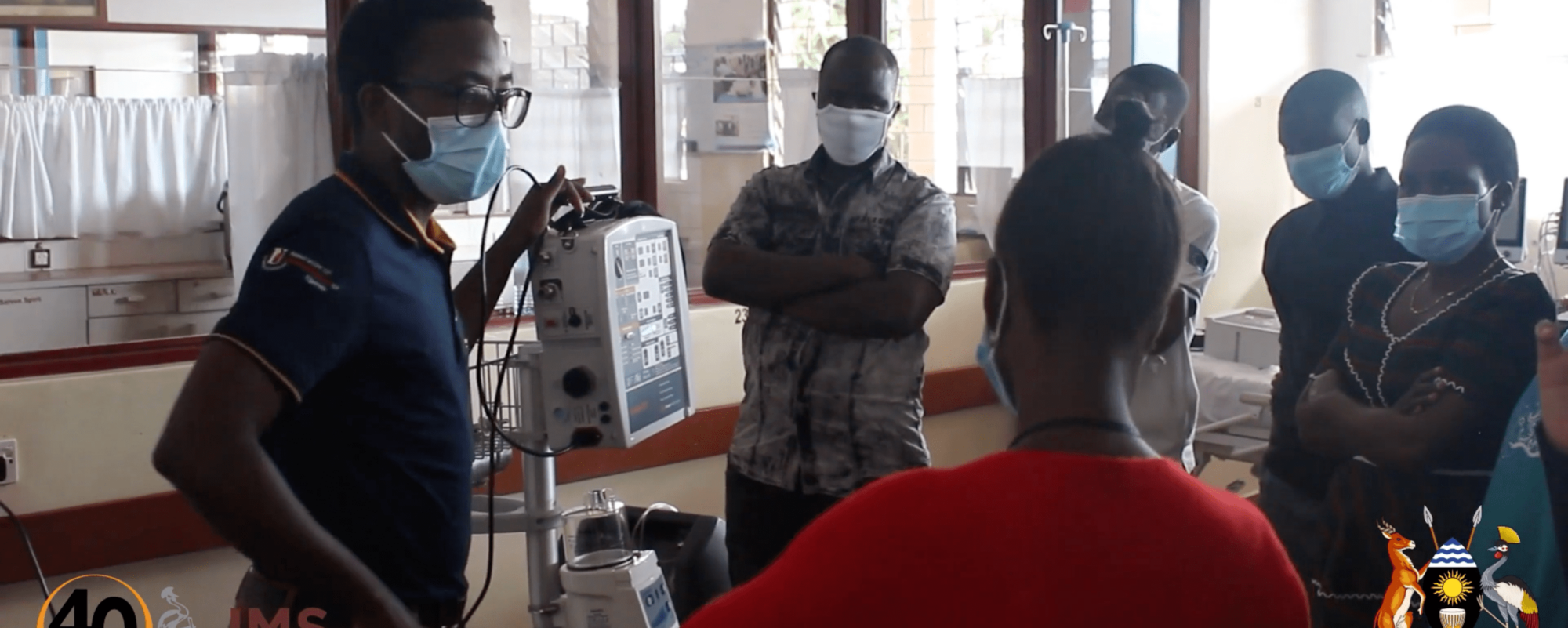
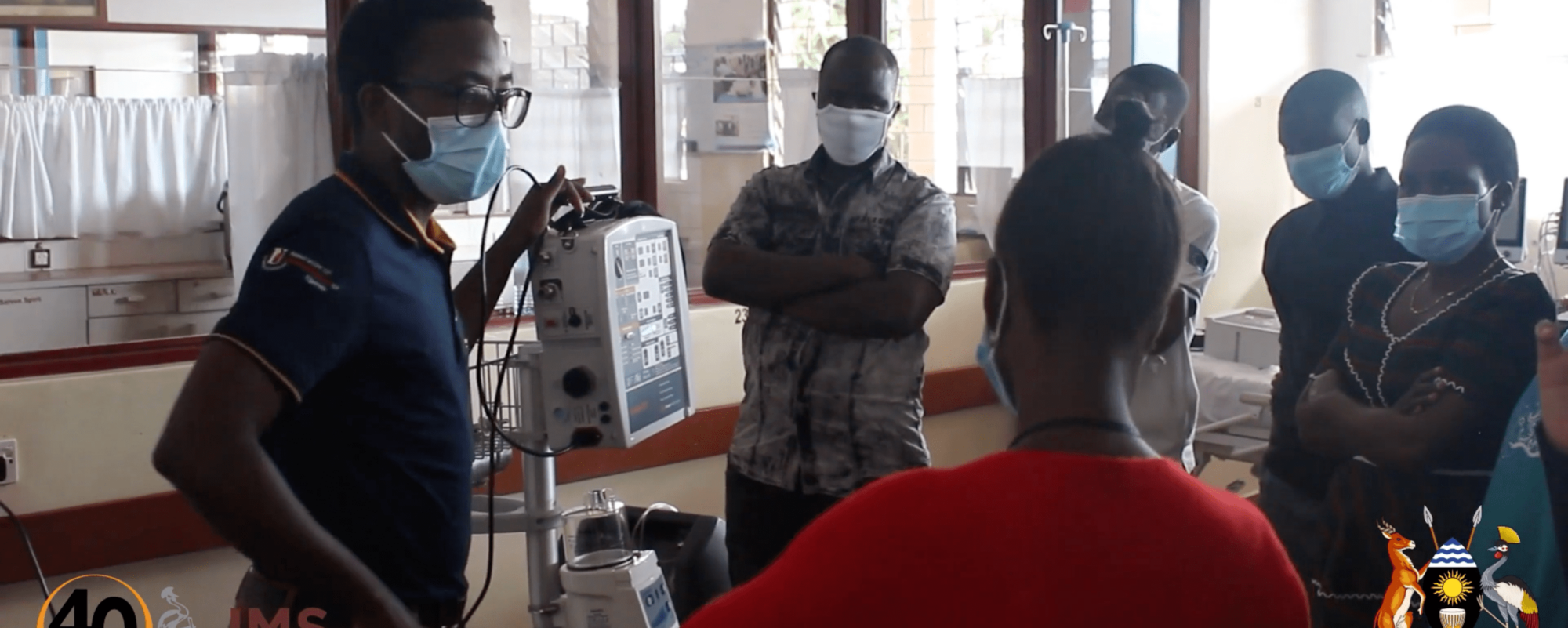
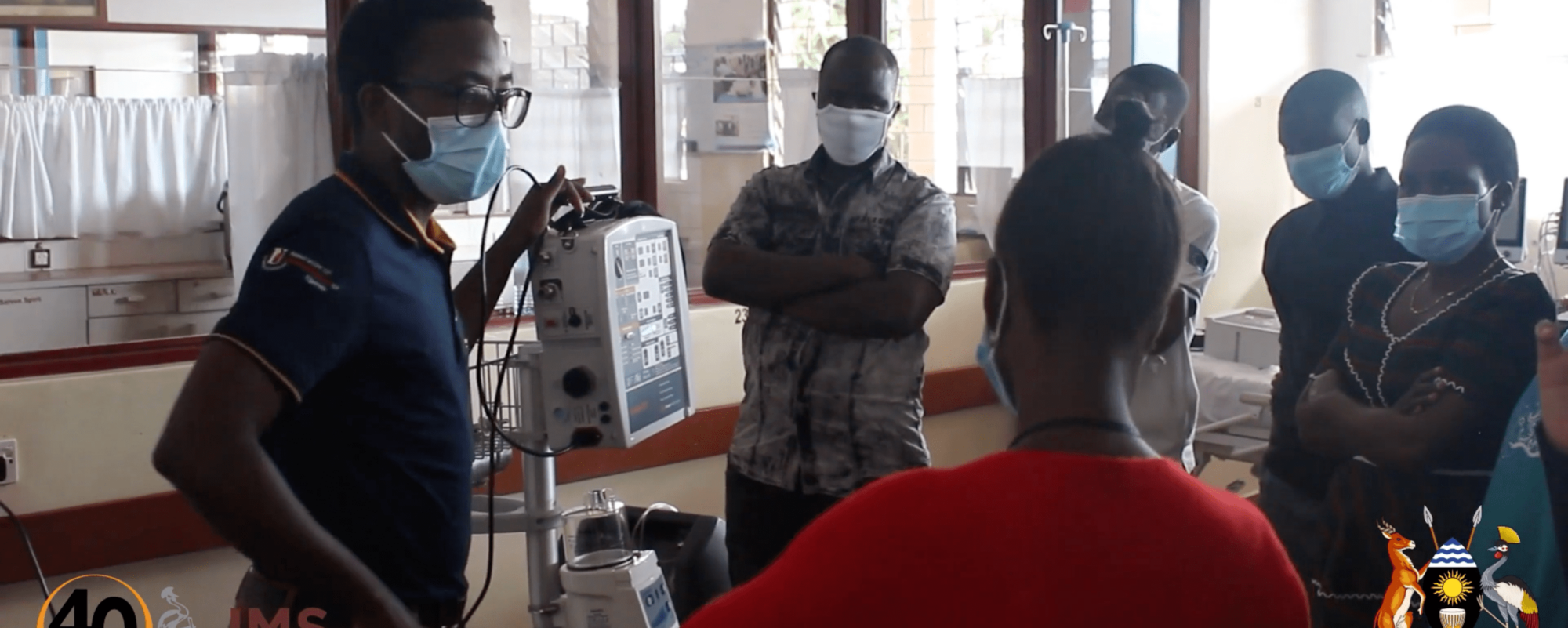
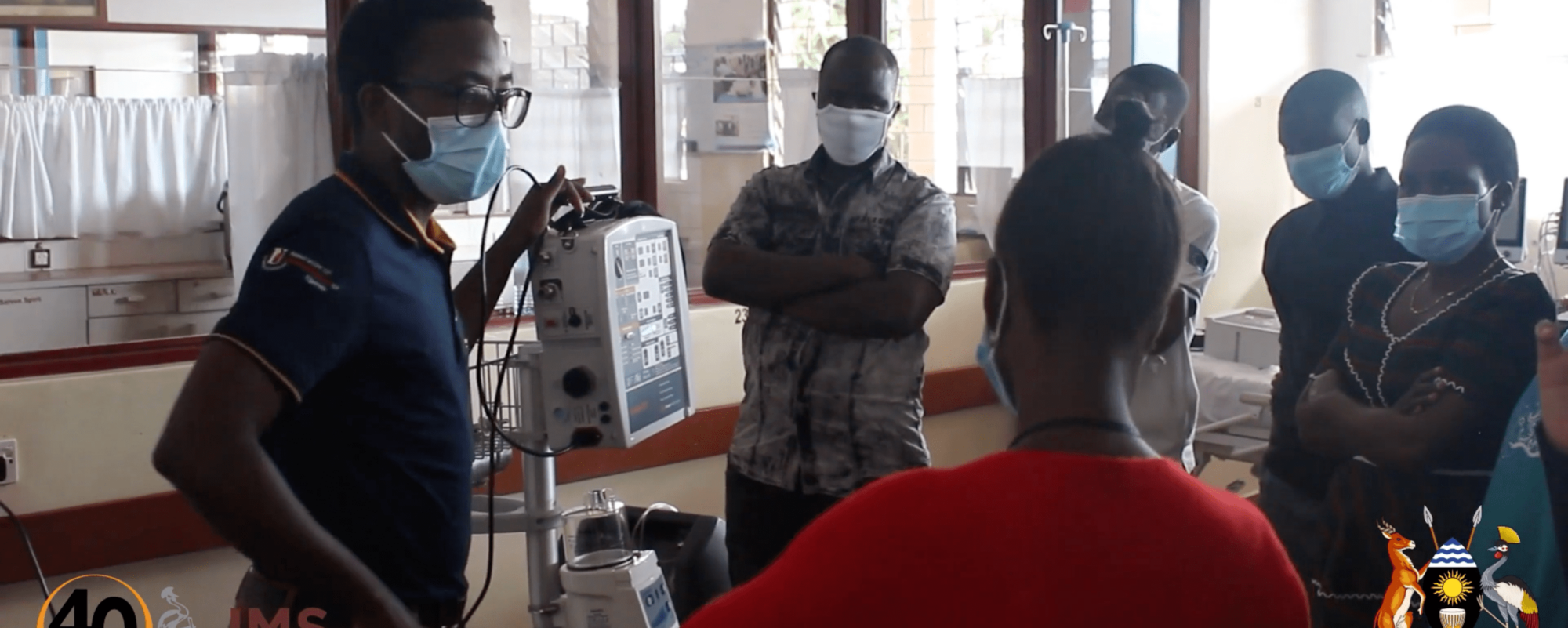
Dr. Fredfly Bulamba is an anesthesiologist working at Busitema University and CURE Children’s Hospital in Uganda and an AAU member. He is also helping lead training activities in support of the government’s national critical care expansion effort. In the video, Bulamba discusses a new training program at regional referral hospitals that blends online and on-site training and staggers training sessions to enable health care providers to learn during their shifts while ensuring care coverage in wards. This training program is being conducted in all regional referral hospitals that have received Gradian CCVs as part of the national government’s ICU expansion effort, and AAU and Gradian are continuing to explore other ways for supporting critical care capacity building efforts in this health facilities and beyond.
Video Transcript:
“This training was developed following the installation [of] the purchase of ICU equipment by the [Ugandan Ministry of Health]. And so we were approached by the Joint Medical Stores and Gradian to design a program that would empower the human resource[s] in the hospitals to provide critical care and use the equipment appropriately. So we designed a curriculum which would look at all the fundamentals of critical care in some important therapies like oxygen therapy. We ran this program as a blended training program, with part of it being covered online or through the virtual environment. We specifically used Zoom, and the rest being run onsite through hands-on, in-person training.”
“We ran this program as a blended training program, with part of it being covered online or through the virtual environment.”
“Our Zoom program worked so well, because we only required our participants to attend for one to two hours each day, continuously for two weeks. And each of those days we would tackle or discuss a different concept for different equipment [in regards to] ICU care. Our main sources of information were the Gradian platform called gradian.learnworlds.com, a global critical care platform called stanesglobal.learnworlds.com, and openpediatrics.org. Following the online training, we’ve embarked on onsite physical trainings where we facilitate anesthesiologists to go out to the regional hospitals that have had their equipment and ICU installed.”
Gradian Training Resource Center
Healthcare providers can use the Gradian Training Resource Center to access easy-to-use product and clinical refresher trainings on anesthesia and critical care that build skills and competency and can fit within a busy schedule.
“They would stay at the hospital for about five days, and have hands-on training on all the ICU equipment and the different basic ICU therapies like oxygen therapy. The onsite training that we’re doing is in such a way that we respect the national guidelines on COVID, but as well as reach a large number of trainees. So we’ve designed the program to run twice a day. We have two sessions, the morning session and the afternoon session. But both these sessions are actually similar. And that means that if a health service provider is providing care on the wards during the morning session, they can come and join that training in the afternoon session, and they will not have missed anything.”
“And that means that we conduct the training but also allow clinical care to continue on the wards. And that’s been very, very helpful. We have an average of 30 participants per hospital: 15 of them would come in the morning, 15 would come in the afternoon, and that training goes on for a whole week. Targeting nurses working in … in the different hospitals; anesthetic care providers; doctors, especially medical officers; and a few physicians have also joined the training. What we realize is that previously as doctors and nurses go through their undergraduate training they have not been well exposed to critical care.”
“And that means that we conduct the training but also allow clinical care to continue on the wards. And that’s been very, very helpful.”
“In every hospital that we’ve trained, we’ve covered the basics of critical care or the fundamentals of critical care. Things to do with definition of what a critical care bed is, what a critical patient needs, and different interventions and therapies that can be provided in a critical care unit. We’ve also trained on therapies like oxygen therapy, fluid therapy. We’ve trained on patient monitors and vital signs monitors. We’ve trained on the ventilators in the units, and specifically, we’ve trained on the CCV, or the Comprehensive Care Ventilator, that’s made by Gradian. We’ve also trained on infusion pumps, syringe pumps, defibrillators and crash carts, among others.”
“We can scale up the knowledge and skill of the healthcare providers, especially the nurses, in actually providing this service. We think that we’ve empowered them to use that equipment appropriately, safely, and make sure that they last for a while. One of the big challenges has been that in every hospital that we’ve gone to almost half of the participants who come for the onsite training did not participate in the initial phase of training which happened virtually. And therefore you find yourself in a situation where you have to provide this training to this individual, but you’re drawn back. The whole group is drawn back to discussing the theoretical part of the training which was covered online.”
“But that’s not entirely bad on its own, because it means that much as people were not able to benefit from the online training, they are still going to benefit from the hands-on training. The other challenge we’ve found is that a lot of our trainees have not been grounded in the basic therapies that we provide in critical care. For example, oxygen therapy, which to many would seem very basic, is not exactly well understood in many of our trainees. And therefore we’ve had to spend a lot more time explaining and teaching on some of the basic things that you would presume people would know.”
“But this is a learning point for us, because we will then plan our trainings even better, knowing that we are really taking our students or our participants from a very basic position to teach them critical care ventilation. Our plan as the Association of Anesthesiologists of Uganda is to make sure that wherever the government has commissioned ICUs, we train the staff there. We train the nurses, we train the medical doctors, and train the anesthetic officers to provide this level of care. But ultimately, we’re continuously interfacing with the government to recruit anesthesiologists into these hospitals, because we do understand that these ICUs will not function effectively without leadership of the anesthesiologists.”
“And therefore, we plan to continue training in all the regional referral hospitals throughout the year, and probably much of the coming year. For now we are running the initial crash course kind of training, but we hope that we’ll be able to find resources to have continuous refresher of the people that we’ve trained in the future. We think that this will be very beneficial to the continuity of running of the ICU service. So our plan is really to scale up [the] training of critical care or exposure of critical care to all trainees that are coming out of medical school and that are coming out of nursing schools. I think in the medium term what we’re going to do is to improve on the content of critical care in the existing curricula.”
“So as the Association of Anesthesiologists, we recognize that this is a very important period in our healthcare system, and it’s an opportunity that we need to take as we work towards improving critical care services in Uganda.”
“But eventually we recognize that we’re going to have to train, formally train critical care nurses and critical care physicians, or specifically anesthesiologists, who will run our critical care units. We also hope that anesthetic officers who are qualified at a virtualized level will also be able to provide care for critical care patients in these units. So as the Association of Anesthesiologists, we recognize that this is a very important period in our healthcare system, and it’s an opportunity that we need to take as we work towards improving critical care services in Uganda.”
“I think we have the mandate to work with the government, to do trainings, to advocate, to get involved in the supply chain, but also advise the government on how best to approach these services.”