
Reaching One Million Surgical Patients
A World Anesthesia Day Update: October 16, 2019


A World Anesthesia Day Update: October 16, 2019

Gradian just reached a major milestone: the UAM has now contributed to more than 1,000,000 safer surgeries worldwide. (Based on our estimates, the UAM’s millionth patient was treated sometime in the middle of 2019.) In a world where 5 in 7 people lack access to safe surgery and anesthesia, the UAM has helped roughly 1,235,000 of them have safer operations, which may not have been possible if the UAM and the ecosystem around it weren’t well-functioning.
As a standalone metric, this figure is certainly important. It is a testament to both the UAM’s durability and the human beings powering its performance in the field. But with the complicated circumstances in which anesthesia is delivered (particularly in low-resource settings), and the dynamic factors affecting the adoption of anesthesia technology, this metric could mean many different things to many different people. Here’s what it means to Gradian:
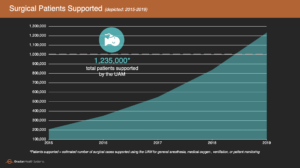
Based on surgical logbook data from more than 50 UAM-equipped operating theaters in sub-Saharan Africa over the course of several years, we have found that the UAM is used for approximately 2.2 surgical cases per day (per UAM, on average), with some variation depending on factors like surgical volume, facility type, workforce capacity, access to drugs and supplies, etc. Extended across our installed base of nearly 700 UAMs–and accounting for when each UAM was installed–this figure translates to 1.235 million surgical cases supported by the UAM since 2011 (and more than 1 million since Gradian spun off as an independent company in 2015).
We also know from anecdotal observations and facility-level data that the most common surgical procedure supported by the UAM is C-sections, particularly at rural health facilities, many of which have been upgraded to provide emergency obstetric care.
It is crucial to note that UAM usage does not necessarily mean that the UAM is used to deliver general anesthesia. In roughly 1/3 of cases, the UAM is used for another function, such as the provision of medical oxygen, ventilation, and/or vital signs monitoring. This use case often accompanies surgical patients under another form of anesthesia, such as local or spinal.
In global health, “lives saved” is the ultimate metric for impact, but it is prohibitively difficult to determine. Attributing a “life saved” to any single medical intervention is often very resource-intensive, particularly in a field like anesthesia, where hundreds of confounding factors contribute to patient outcomes. We recognize that our work exists in a complicated, ever-changing system, and as a result, we prefer to focus on a more reliable scope of observation to understand the impact of our work on patients. If each surgery that the UAM supports represents a patient served, that means that the UAM has enabled safer anesthesia for more than 1.2 million women with childbirth complications, victims of road traffic accidents, children with congenital disorders, and other patients requiring surgery.
Many of these patients would have received inferior care if not for the UAM being present in the operating theater. Some facilities have little to no access to oxygen cylinders, which means their ability to provide inhalational anesthesia hinges on the UAM’s ability to produce its own medical oxygen. Likewise, some facilities experience regular power outages and need the UAM’s unique draw-over mode to deliver anesthesia safely and complete surgical cases that would otherwise be referred, cancelled, or worse. And for an increasing number of hospitals and health centers located in rural parts of sub-Saharan Africa, the UAM is their first source of anesthesia, meaning patients have to travel shorter distances to reach safe care, reducing the risk of adverse outcomes during transport or congestion at higher-level facilities.
But the mere presence of a UAM is not enough to safeguard anesthesia care. For the UAM to serve more than a million patients successfully, it must be both functional and able to be used confidently by the anesthesia provider.
In addition to sheer usage, there are a number of factors that cause medical equipment like the UAM to break down–anything from dust to heat to humidity–which are often exacerbated at health facilities in sub-Saharan Africa with limited resources and difficult environments. At the same time, those who operate specialized medical equipment like an anesthesia machine require specialized training in relevant medical disciplines like anesthesia and critical care. Both of these factors make it essential for medical device suppliers to guarantee reliable service in the field and robust training of clinical users.
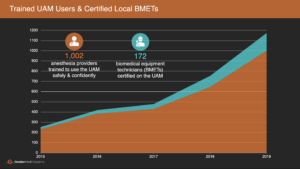
For Gradian, this offering is hardwired into our model and our investment in local capacity to both service the UAM and operate it confidently. Thanks to our partnerships with local distributors in 10+ countries and our new operations hub in Nairobi, Gradian has established spare parts depots to cover all our markets and certified more than 150 local biomedical equipment technicians on our products. Now, we have service representatives in place across the continent to carry out our warranty–which covers on-site preventive maintenance and repair visits, replacement parts, and ongoing remote support–and ensure that all components of the UAM are performing according to spec.

We have also established local infrastructure and partnerships to bring hands-on product training to all our clinical users, wherever they’re based. Since the majority of UAM users are non-physician anesthesia providers, most of whom have a year or less of specialized training, Gradian has invested in simulation-based laboratories and curricula to provide high-fidelity training around key skills and scenarios needed for our users to learn the UAM in the context of their education and experience. We’ve also certified teams of local anesthesiologists and anesthesia residents to lead all UAM trainings. This year, we eclipsed 1,000 users trained on the UAM–almost half whom have completed our simulation-based anesthesia training curriculum.
As innovative and durable as the UAM is, it still requires an ecosystem surrounding it to maximize its effectiveness and sustainability–in other words, the people, products, policies, and processes that make any health system function. At a national scale, this means working in close partnership governments, teaching hospitals, professional societies, service and logistics companies, and local NGOs to make sure that this ecosystem is in place for every UAM and that any program we implement is directed by local institutions. It is also crucial to ensure that this work falls in line with global health priorities, such as maternal and newborn mortality.
In Tanzania, Gradian has partnered with the country’s Ministry of Health, President’s Office, and Medical Stores Department to bring the UAM to nearly 300 rural health centers as part of a national initiative to strengthen comprehensive emergency obstetric and neonatal care (CEmONC). Thanks to partnerships with Muhimbili University of Health and Allied Sciences, Kilimanjaro Christian Medical Center, Bugando Medical Center, Kas Medics, Benjamin Mkapa Foundation, and a host of other Tanzanian institutions, we have mobilized further investments in capacity building for every UAM user in the country.
Here’s a look at the partnership and its early impact on anesthesia care in Tanzania:
We now have a growing body of information on UAM usage from 500+ hospitals around the world, yielding a wealth of insights on the machine and what’s required to get it from factory to facility–and then to keep it running for years on end. We look forward to compiling, synthesizing, and reporting on these insights in the months to come. Stay tuned for more!